So, you’re thinking about designing your own eHealth strategy
Population aging is putting relentless pressure on health systems.
As nations around the world seek to address the challenge of the world’s aging population, they are exploring the ways in which information technology can help them drive healthcare improvements and innovation. We spoke with Asia Pacific, Regional Managing Director for InterSystems, Kerry Stratton, to understand how a premier IT company with a specialty in healthcare IT helps its clients create and implement effective eHealth strategies.
The InterSystems frame of reference is more than 37 years of global health information technology experience, with systems installed in approximately 100 countries. In addition InterSystems’ electronic medical records (EMR) system, TrakCare®, was recently honoured as the “2015/2016 Best in KLAS for Global (non-U.S.) Acute EMR.” Following is what we discussed.
While there is wide variance in political and economic environments, countries face remarkably similar healthcare challenges around the world. A well-designed eHealth strategy is a critical element of the effort to design sustainable healthcare models for the future.
Such a strategy must include a shift from hospital-centric healthcare for individuals to coordinated, distributed health and social care for populations.
A Viable eHealth Model
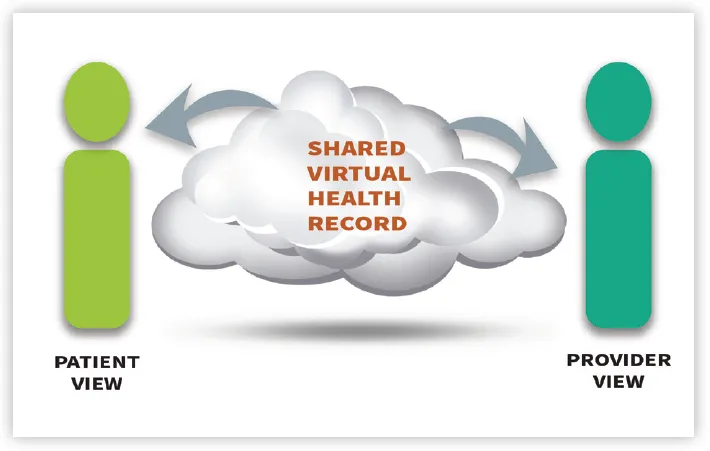
There are four critical elements to an eHealth program. First, the right foundation: the shared virtual care record. In an ideal world, all health and social care providers would work within a unified information system with real-time access to all of the information needed to make sound patient care decisions.
Coordinated care requires an inclusive and comprehensive person-centric record spanning the entire distributed care team, including community healthcare centres, specialists, hospitals, home help, and social care. Similarly, it should reflect the breadth of data types, such as images, medications, notes, test results, and wearable device data.
While many individual healthcare organisations are moving toward a unified EMR, spurred on by patient safety and efficiency drivers, this kind of monolithic environment is not possible across a care continuum involving a growing array of disparate organisations.
The community-wide model has different stakeholders, regulatory context, processes, IT systems, and often funding. Consider, for example, the need to incorporate social services such as child protection into a community care process; these providers do not and will not use an EMR, yet they need to be able to connect all the dots for a given patient.
A comprehensive virtual care record aggregates information from all sources and participants, including the patientnormalises that record-and makes it available in a relevant format to each member of the care team in the appropriate workflow.
Second, the right tool for the job: agility at the point of service. Optimal population health management requires safe, high-quality care for every individual, so every member of the virtual care team needs the best technology for his or her role. For healthcare professionals, this is a comprehensive EMR.
For social care providers, it may be a registry or case management system. But it must provide everyone with access to the shared virtual care record. Assuming the foundational, shared virtual record is in place, clinical providers can choose an acquisition approach most suited to local priorities, relationships, and funding.
Regardless of the approach, all clinical team members must ultimately have the information they need to deliver care efficiently, adopt best practices, and communicate effectively.
Third, do the right thing: the shared care plan. We all want to do the right thing for the health of our communities. But given the distributed nature of the care team, the need for close communication, and the rapid introduction of new diagnostics and therapies, it is nearly impossible to keep everyone adequately informed without technological assistance.
Responsibility for this coordination can be unclear and technology to enable it lacking. Within the hospital walls, integrated treatment pathways drive order sets within an EMR for a physical care team.
Complementing these, clinical decision support and alerting functionality reduce medication errors, assist with selecting optimal therapies, and warn of possible gaps in care. Out in the community, the distributed care team needs a shared care plan, built on the shared virtual care record.
Fourth, the right focus: actionable analytics. The accounting truism that “what gets measured gets managed” applies to healthcare and is the reason why quality and performance measures have become widespread in healthcare systems around the world. The term “analytics” is used to describe a diverse mix of approaches, ranging from simple management reports to complex predictors of the risk of death from a specific condition.
The shared virtual record
The shared virtual record should include embedded analytics capabilities that support reporting, metrics, and dashboards at a minimum, as well as monitor and document improvements in both outcomes and utilisation. It may also support risk stratification and predictive models, or be used as a near real-time data source for specialised analytics applications.
If you are ready to design or enhance your own eHealth strategy, consider developing a plan that includes these steps:
Step 1: Document the starting point. Identify and begin gathering baseline metrics related to the goals of your eHealth initiative. You may have only limited data available at this stage, but this baseline will enable you to measure and accelerate successes.
Step 2: Create the connected health record. Start by examining the EMR strategy within your organisation to identify risks and the gaps in seamless care provision. The EMR will continue to be the centre of the universe for patient data, but that universe is expanding.
Step 3: Foster patient and provider engagement. Create outreach programs and peer champions to encourage providers, patients, and families to adopt and embrace the shared virtual record and care plan as an integral part of their own care management processes.
Step 4: Enhance the EMR. Whether you adopt a single community-wide EMR or multiple different systems, implementing next-generation EMR technology requires careful planning and change management. The shared virtual record provides the necessary archival repository to ensure continuity, and it insulates caregivers from the impact of that change, as older data sources are swapped out and replaced.
Step 5: Measure-Monitor-Improve-Repeat. At each step along the path to a mature eHealth program, there will be opportunities to enhance and improve care processes, drive efficiencies, enhance patient satisfaction, and learn from experience. The essence of a learning health system is continuous measurement and improvement.
Mr Stratton concluded, “Nations everywhere are facing the realities of a new healthcare environment — one in which healthcare is a team activity, patients are equal partners in the care continuum, and new approaches are needed to ensure sustainable funding for increased demands. An eHealth model designed for this new environment spans the entire community, engages patients, reduces costs, and improves outcomes.”
If you have any questions regarding the content of this article, or would like to learn more, please contact Kerry Stratton via www.InterSystems.com/HealthCareAsia


















 Advertise
Advertise






