Hybrid infrastructure accelerates healthcare AI adoption
APAC providers turn to hybrid models to scale AI securely.
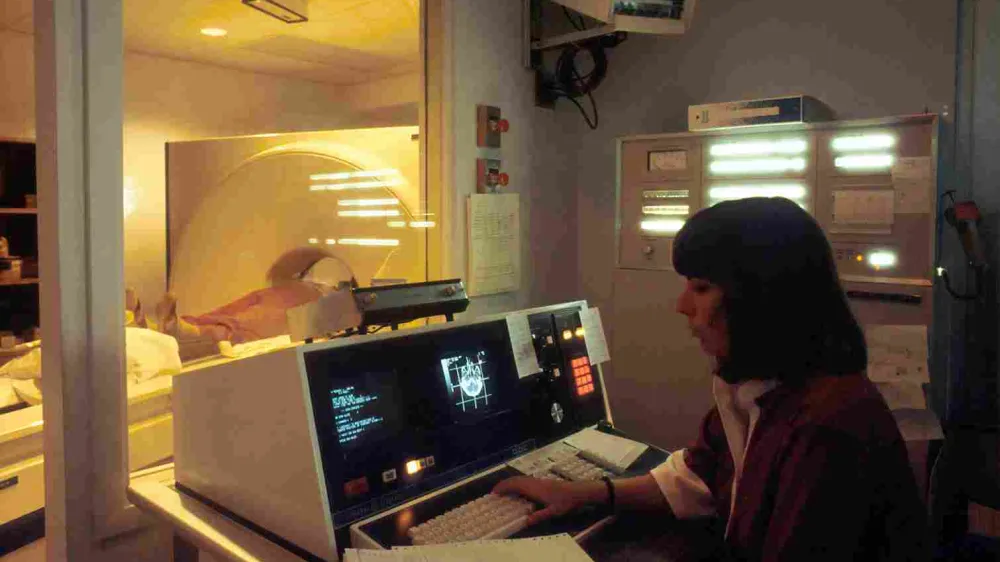
Healthcare providers across Asia Pacific are accelerating adoption of artificial intelligence as hybrid infrastructure becomes the preferred foundation for scaling diagnostics, patient services and operational efficiency while managing rising data volumes and security risks.
Lenovo’s CIO Playbook 2025 shows that 65% of organisations now favour hybrid AI and high-performance computing environments, reflecting the need to balance strict data sovereignty requirements with the scalability of cloud-based AI. The shift comes as healthcare data volumes surge, with the sector generating roughly 30% of global data and forecast to grow nearly 40% year on year through 2026 and 2027.
Sinisa Nikolic, Director and Segment Leader, HPC & AI, Asia Pacific, Infrastructure Solutions Group at Lenovo, said hybrid infrastructure aligns with the regulatory and operational realities of healthcare. “It really is an ideal mix,” he said. “You can keep clinical and patient data on premise… because clinical data, patient data, personal data, needs to meet some very, very strict compliance regulations.” At the same time, he said, hybrid models allow providers to use the cloud “for more scalable AI, collaboration, faster innovation,” adding that “not moving data will save money.”
David Irecki, Chief Technology Officer of Boomi, said hybrid adoption is becoming unavoidable as care models evolve. However, he warned that hybrid environments introduce complexity. “That's why a unified integration layer becomes essential,” Irecki said, noting that fragmented systems slow real-world deployment. “Healthcare isn't slowed by AI models. It is actually slowed by fragmentation, and that remains the biggest bottleneck.”
That fragmentation is preventing providers from moving beyond pilot projects. Irecki cited regional research showing that “across APAC, only 30% of workflows are optimised for generative AI at scale.” He added that progress depends less on new algorithms and more on integration. “The next breakthrough in healthcare won't come from a new model. It'll actually come from connecting the models that we already have today,” he said.
Nikolic said many organisations are still not prepared for enterprise-wide AI. “A lot of healthcare organisations today simply aren't data ready,” he said. “Data is fragmented. It's reasonably inconsistent. It's not governed well.” He added that legacy infrastructure often cannot support the compute and storage demands driven by AI, while the absence of cross-functional sponsorship slows deployment.
As AI adoption expands, operational risk is rising sharply. Nikolic warned that AI introduces new threats, including “data poisoning, model drift, unvalidated outputs,” which can undermine clinical decisions even without a breach.
In hybrid environments, where AI interacts with on-premise and cloud systems, Irecki said oversight is critical. “Ultimately, AI should return time to clinicians, not add risk,” he said.

















 Advertise
Advertise





