
Agentic AI to unlock $120m in healthcare system savings
The tool encompasses patient interactions and end-to-end administrative processes.
Healthcare systems that will use agentic artificial intelligence (AI) in healthcare revenue cycle management (RCM) tools could gain $60m to $120m in savings and $6b in revenue, McKinsey & Company said.
According to McKinsey analysis, using AI to enable the revenue cycle could lead to a 30% to 60% reduction in cost to collect, faster cash realisation, and a workforce refocused on patient value rather than administrative tasks.
In 2025, it added that more than 30% providers prioritised the implementation of AI and automation for seven specific use cases across the revenue cycle, compared with four to five use cases in 2023 and 2024, respectively.
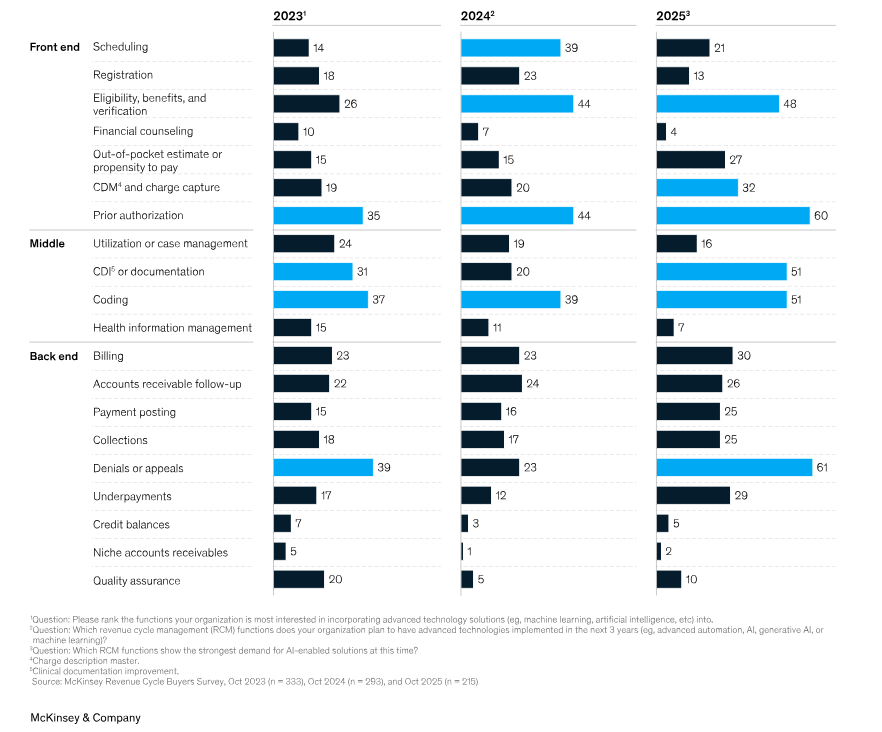
RCM leaders showed the strongest demand for AI-enabled front-end solutions in 2025 is prior authorisation, with 60%, the consulting firm’s data showed.
The year before, 44% of RCM functions planned to use AI-enabled prior authorisation in the next three years.
In the middle-end, client documentation improvement (CDI) showed the highest demand for the tools during the year. Demand here stood at 20% the year before.
For AI back-end functions, 61% of demand in 2025 was recorded by denials or appeals, of which 23% planned to implement the AI the previous year.
For patients, agentic AI in RCM could result in faster access to care and more streamlined billing, McKinsey said.


















 Advertise
Advertise






